What is Amyotrophic Lateral Sclerosis ?
Amyotrophic lateral sclerosis (ALS) is a serious neurodegenerative disease that selectively affects motor neurons responsible for controlling voluntary movements. As these neurons in the brain and spinal cord cease to function, patients develop progressive muscle weakness leading to paralysis, along with difficulty speaking, swallowing, and even breathing. Senses and intellectual function usually remain intact, but the loss of muscle control worsens over time. Half of those affected die within 3 to 5 years of the first symptoms, often due to respiratory failure.
Currently, there is no cure for ALS, and available treatments are very limited. The most commonly used drug, riluzole, can slightly prolong patients' life expectancy by slowing disease progression, but its benefit is modest and does not stop functional decline or significantly improve quality of life. Another approved medication is edaravone, an antioxidant that reduces neuronal oxidative stress, which showed a slowing of functional decline in clinical trials. However, current treatments generally only alleviate symptoms or slightly delay the progression of ALS. This lack of effective therapies makes it urgent to investigate new therapeutic strategies to slow or stop the disease. Below, we review some of the most promising research lines under development.
New therapies in development
Faced with the limitations of conventional therapies, the scientific community is exploring various innovative options for treating ALS. Among the main lines of research are gene therapies, the use of stem cells, immunotherapies, and the development of small molecules targeting pathological processes of the disease (such as inflammation or oxidative stress). Below, we describe these strategies in an accessible yet rigorous manner.
Gene therapies: Custom genes against ALS
One of the most innovative approaches is gene therapy, which aims to correct or counteract genetic defects by introducing therapeutic genetic material into the patient's cells. In the context of ALS, this can involve two approaches: providing functional copies of protective genes or silencing harmful mutated genes. Viral vectors (modified viruses serving as "vehicles" for the therapeutic gene) capable of delivering genes or RNA fragments to motor neurons are often used for this purpose. For example, in hereditary forms of ALS caused by known mutations, vectors delivering instructions to inactivate the mutated genes are being tested.
A notable case is tofersen, an antisense oligonucleotide designed for a type of familial ALS with a mutation in the SOD1 gene. Tofersen is administered directly into the cerebrospinal fluid (intrathecal route) and reduces the production of the mutant SOD1 protein, associated with motor neuron death. Clinical studies have shown that tofersen decreases a biomarker of neuronal damage (neurofilaments) and, although its clinical effects are still being evaluated, it has generated hope and was recently approved for patients with the SOD1 mutation.
In addition to antisense oligonucleotides, trials exist with adeno-associated viruses (AAV) and other vectors to deliver therapeutic genes. For instance, research is investigating the introduction of genes encoding neurotrophic factors (proteins promoting neuron survival) or interference RNA that block other toxic molecules implicated in ALS. Although still in early stages, these gene therapies offer an approach targeted at the molecular root of the disease, with the potential to alter its course rather than just treating symptoms.
Stem cell therapies: Regeneration and support for neurons
Another strategy under development is cell therapy, using stem cells to protect or replace damaged motor neurons. Mesenchymal stem cells (MSCs), typically obtained from bone marrow or adipose tissue, are particularly investigated due to their immune modulation capacity and secretion of trophic factors (molecules promoting tissue repair). The general idea is that transplanting these cells into the patient (either into the spinal cord, muscles, or intravenously) can create a more favorable environment for remaining motor neurons: reducing inflammation, releasing growth factors, and perhaps differentiating into support cells (like glial cells) that help keep neurons alive. The goal is not to directly "replace" lost motor neurons, but rather to slow or stop ongoing degeneration.
In animal models of ALS, various cell therapies have shown delayed disease progression. In humans, pilot clinical trials have been conducted: for example, infusions of MSCs into cerebrospinal fluid or injections into muscles. Some small, uncontrolled studies suggest they might slow ALS progression in certain patients. However, results from more rigorous randomized trials have not yet shown conclusive benefits, and no stem cell therapy is currently approved for ALS.
Despite this, cell therapy is a very active field. Biotech companies and academic groups (in Europe, the US, and other countries) continue to recruit patients for studies with MSCs or other cell sources (such as neural stem cells) aiming to confirm their safety and efficacy. The hope is that, combined with other interventions, stem cells could prolong survival or stabilize muscle function in ALS. Every advance in this area is closely watched, as it would offer a completely new therapeutic option based on regenerative medicine.
Immunotherapy: Antibodies slowing degeneration
Given that inflammatory processes and the accumulation of abnormal proteins are involved in ALS, another line of research is immunotherapy, which uses monoclonal antibodies or other immune system strategies to combat the disease. One approach is to develop antibodies targeting toxic proteins that accumulate in motor neurons (such as abnormal aggregates of TDP-43 or SOD1), so the immune system itself helps eliminate them. Another strategy is to target antibodies against immune system molecules that mediate inflammation in the nervous system.
For example, microglia cells (the brain's immune defense) can become hyperactive in ALS and contribute to neuronal damage. In a recent study, scientists identified a protein called integrin alpha-5 on immune cells in the nervous system of ALS patients and tested a monoclonal antibody against this protein in a mouse model of the disease. The results in mice were promising: the treatment protected motor function, delayed ALS progression, and even prolonged the animals' survival. This antibody (originally developed for certain types of cancer) could potentially be repurposed for ALS, accelerating its path to human clinical trials.
Beyond this case, trials are underway with immunotherapies, such as anti-TNF antibodies (a pro-inflammatory cytokine) or inhibitors of other immunological pathways (e.g., anti-TREM2 or anti-CD14 antibodies, targeting modulators of microglial activation). The administration of immunoglobulins and other forms of immunomodulation to reduce neurotoxic inflammation is also being explored. While immunotherapy in ALS is still in its early stages, advances in other neurodegenerative diseases (like the recently approved antibodies for Alzheimer's) provide reasons for cautious optimism. Controlling the maladaptive immune response could slow damage to motor neurons, complementing other therapies targeted at the neurons themselves.
Small molecules: Curbing inflammation and oxidative stress
In addition to gene, cell, or antibody therapies, the search continues for small molecule drugs—traditional chemical compounds—that can alter the course of ALS. Various clinical trials are investigating drugs with different mechanisms of action, including: reducing inflammation, blocking cell death due to oxidative stress, or improving neuronal metabolism.
An example already mentioned is edaravone, a free radical scavenger (antioxidant) that alleviates oxidative stress in neurons. Edaravone demonstrated a reduction in the rate of functional decline in patients over 6 months compared to placebo, leading to its approval in 2017 (as Radicava), becoming the second FDA-approved drug for ALS in 22 years. Another novel drug is AMX0035 (a combination of sodium phenylbutyrate and taurursodiol), which acts by protecting the mitochondria and endoplasmic reticulum of the neuron; this compound showed prolonged survival in trials and was approved in 2022 in the United States and Canada.
Regarding inflammation, one of the most prominent experimental drugs is masitinib, a tyrosine kinase inhibitor that modulates the activation of immune cells (like mast cells and microglia) involved in neuroinflammation. A clinical study in nearly 400 patients reported that, when added to riluzole, masitinib reduced the rate of functional decline by 27% compared to placebo after 48 weeks. This result is encouraging and has prompted conditional approval applications in Europe. However, its long-term safety and efficacy are still under careful evaluation.
Other compounds under investigation include: drugs regulating protein homeostasis (like arimoclomol, which induces molecular chaperones to handle misfolded proteins), ion channel inhibitors that may alleviate motor neuron hyperexcitability, and various oral anti-inflammatories or immunomodulators. While each molecule alone usually provides modest benefit, the future goal might be to combine several treatments (e.g., gene therapy + drug + cell support) to attack the disease from different angles. Given the complexity of ALS, every "small" pharmacological advance is valuable, and several of these compounds are in the final stages of clinical trials awaiting confirmation of their results
Manufacturing and TECNIC's role in new therapies
Developing these innovative therapies for ALS involves not only scientific and medical challenges but also manufacturing hurdles. Unlike traditional chemically synthesized drugs, many of these new therapies are complex biological products (genes, cells, viral vectors, proteins) requiring sophisticated production processes and strict quality controls. In this context, bioprocessing technologies play a critical role in bringing therapies from the lab to clinical and industrial-scale production.
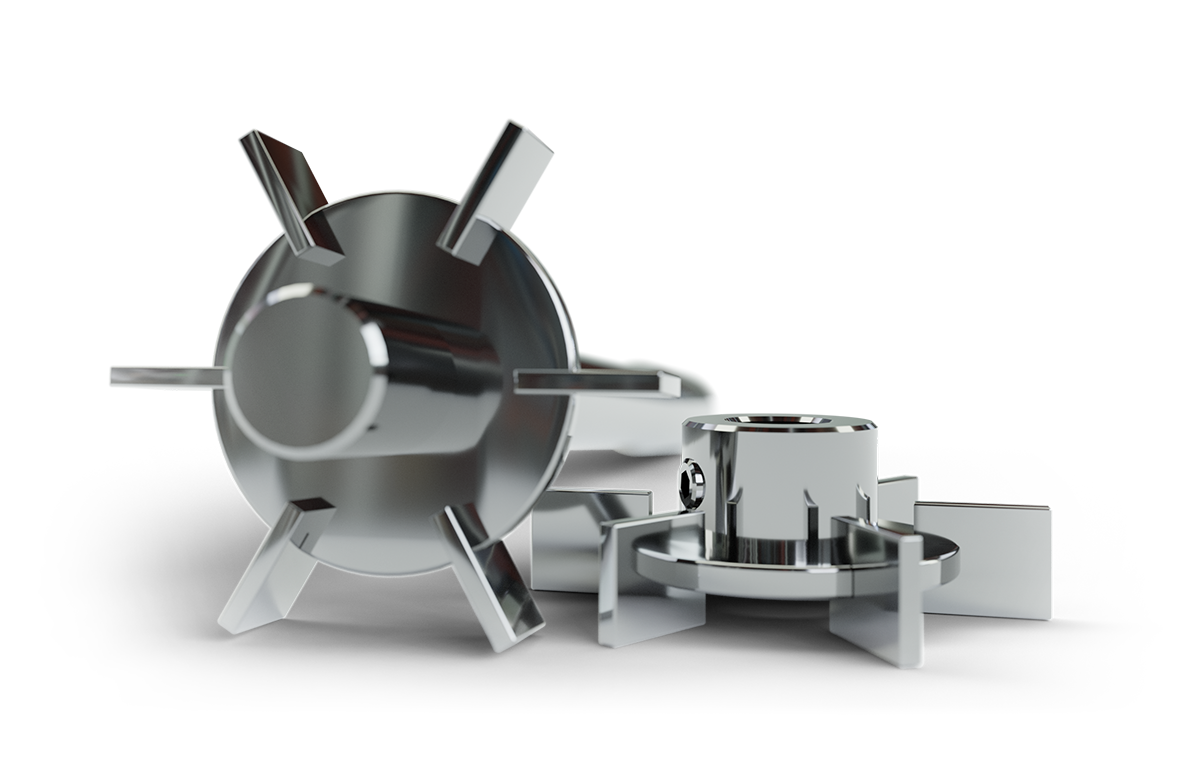
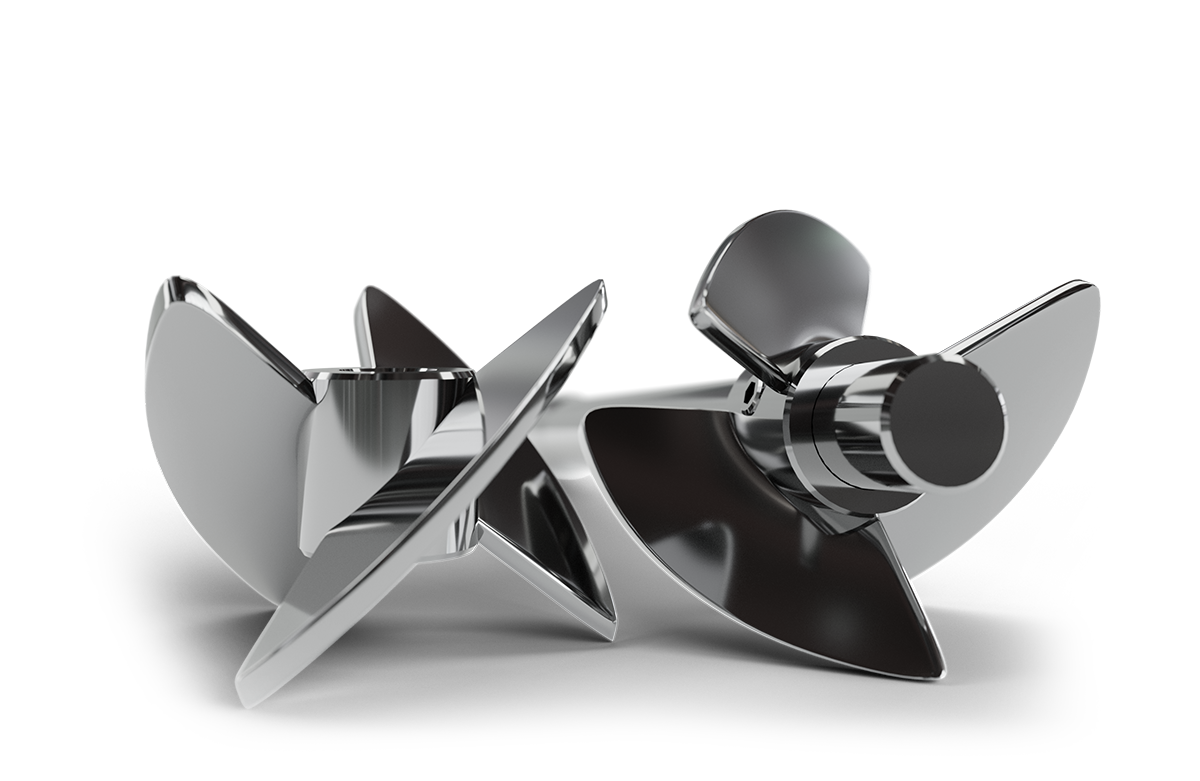
For example, in gene therapy, the core of the treatment is a viral vector (like an adenovirus or adeno-associated virus) carrying the therapeutic gene. Viral vector production is a complex process involving culturing cells (usually human cells or embryonic kidney cells, HEK293, etc.) in which recombinant viruses are generated. This large-scale cultivation is performed in bioreactors, which provide optimal conditions (nutrients, pH, oxygen, temperature) for cells to produce large quantities of the vector. Once the viruses are "harvested" from the cell culture, an equally important step follows: purification and concentration.
Here, tangential flow filtration (TFF) is indispensable, a filtration technique where the solution containing the viruses flows parallel to a membrane, allowing separation of particles by size. TFF is used in almost all biopharmaceutical processes to concentrate viral particles or proteins. Thanks to tangential filtration systems, it is possible to remove impurities and obtain highly purified viral vectors while maintaining their integrity and functionality. Finally, a gene therapy product ready for formulation and patient administration is achieved, meeting required quality standards.
In the case of stem cell therapies, the challenge is to expand a sufficient number of cells with therapeutic characteristics, maintaining their potency and viability. Treating ALS patients (or those with other diseases) may require billions of cells per batch. This is unfeasible using traditional methods of culturing in plates or lab flasks. Therefore, specialized bioreactors are used that allow large-scale cell cultivation in a controlled manner. Bioreactors provide a stable and sterile environment where stem cells can proliferate exponentially. These closed, automated platforms ensure precise control of parameters such as cell density, nutrients, gases, and growth factors. In fact, bioreactors are the preferred platform for controlled cell expansion, offering numerous advantages: reducing manual labor, improving the homogeneity of produced cells, and increasing expansion efficiency compared to plate methods.
Equipment like single-use bioreactors, which use pre-sterilized disposable bags or containers, also provide flexibility and speed by avoiding cleaning steps between batches and facilitating production scaling according to demand. In the manufacturing of cell therapies for ALS, these systems allow obtaining mesenchymal stem cells in large quantities ready for clinical delivery, complying with Good Manufacturing Practices (GMP).
In all these cases, technology provided by specialized companies is essential. TECNIC, for example, offers advanced bioreactors (from lab scale to industrial production) and fully integrated tangential flow filtration systems, designed to meet the rigorous requirements of these innovative therapies. This equipment allows precise automated control of cultivation and filtration conditions, ensuring reproducible and scalable processes.

Frequently Asked Questions (FAQ)
A progressive neurodegenerative disease that affects motor neurons, leading to muscle weakness and paralysis.
No, there is currently no cure. Existing treatments only slow disease progression slightly.
Gene therapy, stem cell therapy, immunotherapy, and small molecule drugs.
Not directly. They help by reducing inflammation and supporting surviving neurons.
It targets genetic mutations or introduces protective genes using viral vectors or antisense oligonucleotides.
References
- Miller, T. M., Cudkowicz, M. E., Genge, A., et al. (2022). Trial of Antisense Oligonucleotide Tofersen for SOD1 ALS. New England Journal of Medicine, 387, 1099–1110.
- European Medicines Agency. (2024). Masitinib AB Science: Public Assessment Report.
- U.S. Food and Drug Administration. (2022). FDA Approves Oral Form of ALS Treatment.
- U.S. Food and Drug Administration. (2017). FDA Approves Drug to Treat ALS.
- U.S. Food and Drug Administration. (2022). RADICAVA® (edaravone) Injection, for Intravenous Use.
- European Medicines Agency. (2024). Meeting Highlights from the Committee for Medicinal Products for Human Use (CHMP) 14-17 October 2024.
- Nature Neuroscience. (2025). Endothelial TDP-43 Depletion Disrupts Core Blood–Brain Barrier Functions.
- Nature Communications. (2024). Adeno-Associated Virus as a Delivery Vector for Gene Therapy of Neurological Disorders.
- National Institutes of Health. (2023). Advances in ALS. News in Health.
- VHIR - Vall d'Hebron Institut de Recerca. (2024). Vall d'Hebron participates in an international study to validate the drug masitinib for the treatment of amyotrophic lateral sclerosis.
- ALS Association. (2025). Medications Approved to Treat ALS. ALS Association.
- National Institutes of Health. (2023, February 28). Identifying potential treatments for ALS. NIH Research Matters.